Summer is one of the most liberating seasons, a time to really let your hair down and enjoy the sunshine. From weekend getaways and outdoor concerts to full-blown music festivals, it's hard to resi...

Is Intermittent Fasting Secretly Sabotaging Your Hair? Intermittent fasting is all the rage these days on social media, hailed for everything from weight loss to reduced risk for Alzheimer's diseas...

The human immune system is a marvel of biological engineering, a silent and sophisticated network of defence molecules that work tirelessly to neutralise external threats like viruses and bacteria ...

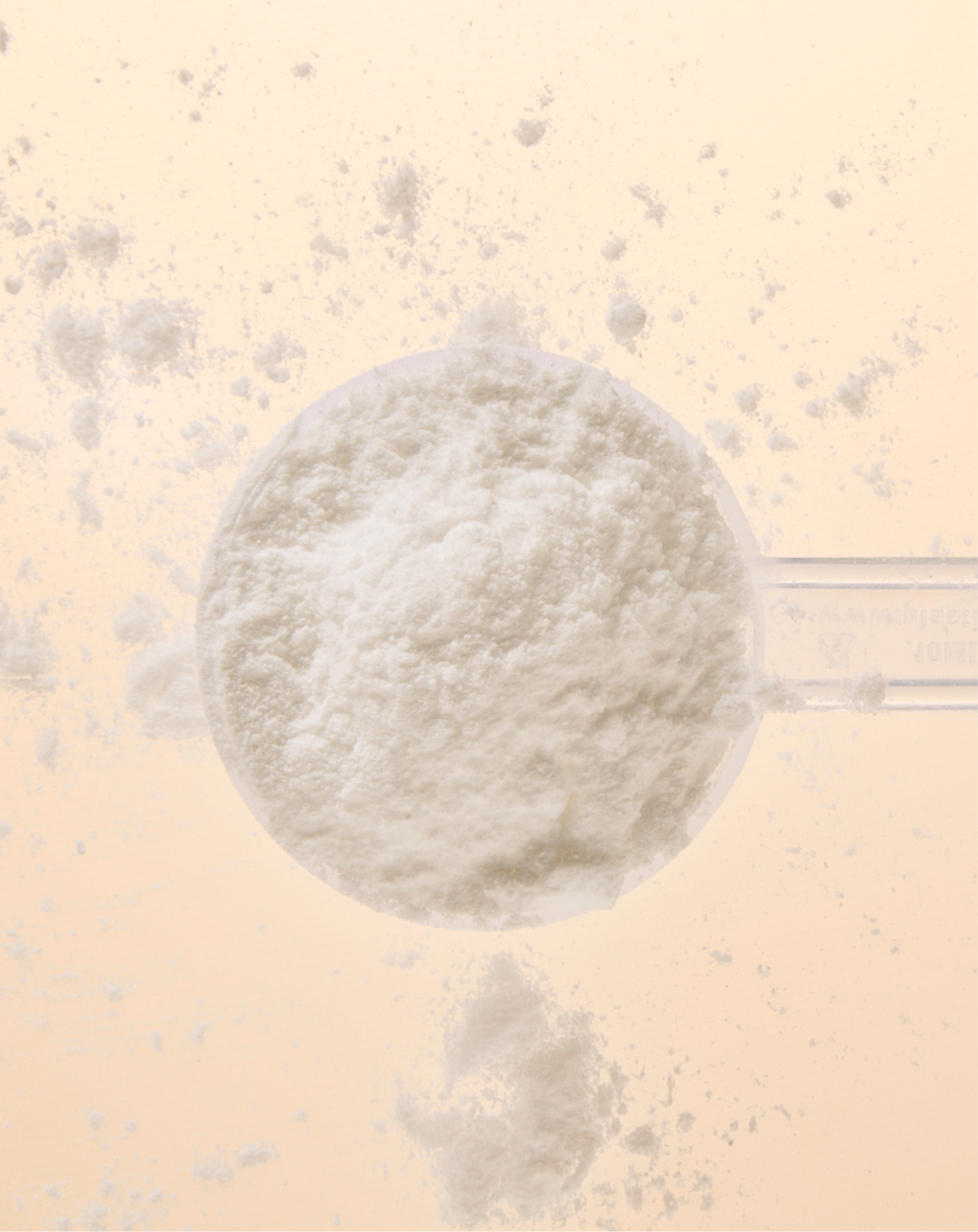
We’re thrilled to introduce Neutrient Advanced Creatine, the newest innovation in our supplement lineup. With so many creatine options available, choosing the right one can be overwhelming—that’s w...

Creatine Monohydrate is a widely recognized dietary supplement, particularly valued in the sports and fitness industry. Athletes and fitness enthusiasts use it to enhance athletic performance, supp...

Vitamin D is often dubbed the “sunshine vitamin,” but this commonly used term only tells half the story. While it’s true that our bodies can make vitamin D when exposed to sunlight, many people are...

How to Energise Your Brain With age, you may notice changes in your energy levels and mental sharpness. Although this is common, it's not an inevitable part of growing old. Many people who stay act...

According to the World Health Organization, 1 in 6 people worldwide will experience infertility at some stage in their lives.1 As more individuals seek out natural ways to improve their chances of ...

Marathon day is approaching, and if you’re one of those fitness enthusiasts hoping to cross the finish line in good time, you’ve probably already spent weeks pounding the roads. But are you on top ...

Author: Jacqueline Newson BSc (Hons) Nutritional Therapy Edited by: Alejandra Toro, Pshychologist, MSc Nutrition and Behaviour Histamine - The Main Offender If you are prone to hay fever, your bo...

Spring is the season of renewal, making it the perfect time to refresh your health and wellness routine. With longer days and brighter mornings ahead, why not embrace the season by indulging in del...

How Poor Sleep Affects Your Skin There are over 90 recognized sleep disorders, many of which impact skin health due to their effects on hormone regulation and stress levels.2 Sleep regulates essent...

Written by: Jacqueline Newson BSc (Hons) Nutritional Therapy As spring approaches, it's only natural to feel inspired by the season's cycle of growth and renewal - a perfect opportunity to let go o...

As we step into a new year, many people are looking to get back into fitness—whether it's to feel stronger, improve energy levels, or simply maintain a healthy, active lifestyle. But jumping into i...
Written by: Jacqueline Newson BSc (Hons) Nutritional Therapy After the Christmas festivities, many of you may feel sluggish, bloated, and out of sync. While the holidays are a time for indulgence a...